Endodontic treatment, i.e. a root canal, is one of the most common dental procedures performed with well over 14 million completed every year. Endodontic treatments have very high success rates (90%-95%), and are completed to help patients retain their natural teeth and avoid tooth extraction.
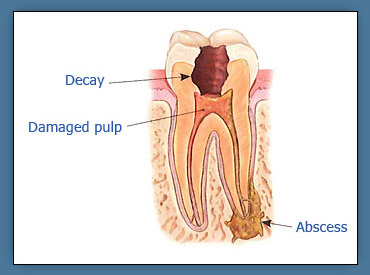
At the center of your tooth is the dental pulp, a collection of blood vessels, nerve fibers, and connective tissue. The pulp once helped form your tooth and continues to supply it with nutrients and defense mechanisms against bacteria and germs. However, if these harmful bacteria invade the pulp by way of a large cavity, trauma, cracks or chips, or repeated but necessary dental procedures, the pulp can become highly inflamed and possibly infected.
Symptoms of an inflamed or infected pulp vary, but include pain to hot or cold, pain when chewing, a spontaneous or constant toothache, or swelling of the surrounding soft tissues. Once your tooth has been diagnosed with an infected pulp, your dentist will most likely recommend root canal therapy in order to remove the diseased tissues.
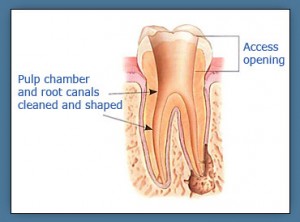
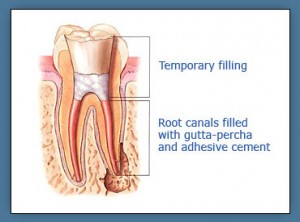
The root canal procedure itself is performed under local anesthesia. Nitrous oxide can also be used if indicated. A small cavity is prepared in the crown of your tooth that allows us access to the diseased pulp within the roots. With advanced instrumentation techniques, the inflamed pulp is removed and the root canal system is thoroughly cleansed and sealed. For most cases this can be completed in a single visit. In certain cases of higher complexity or more advanced disease, a second visit may be indicated to best treat your tooth.
| Step One | Step Two |
 |
 |
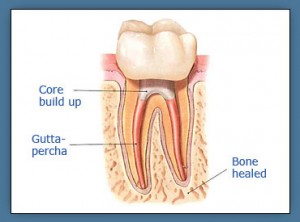
Following root canal therapy, you will need to return to your dentist for a final filling or placement of a crown. A follow up visit to our office at 6 months and/or 1 year is usually indicated to monitor and ensure proper healing.
| Step Three |
 |